Inflammatory bowel diseases (IBD) such as colitis and Crohn’s disease affect more than a million individuals in the United States alone. These conditions cause painful inflammation in the digestive tract and make processing food difficult for the afflicted. However, the impact of these diseases goes beyond the digestive system. Research suggests that inflammatory bowel diseases also affect bone marrow, opening up possibilities for more comprehensive treatment options to help people cope with these ailments.
At present, conventional treatment options for IBDs like Crohn’s and colitis are mostly non-preventive measures, such as the prescription of steroids and narcotics to manage inflammation and pain. In more severe cases, surgeries to remove parts of the digestive tract may be necessary. However, these treatments offer meager relief from the primary conditions and present significant risks of degenerative tissue damage.
The Link Between Bone Marrow and IBD
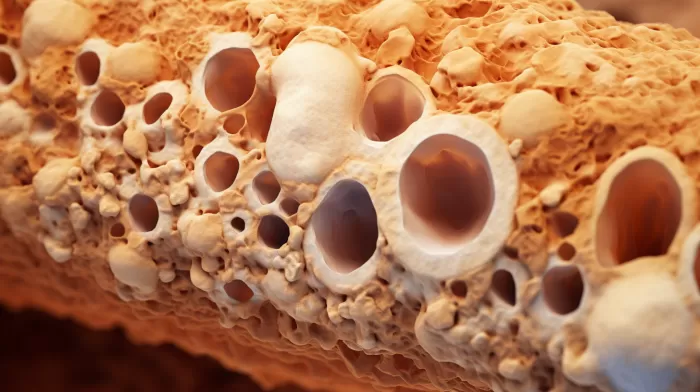
A study by researchers from Michigan State University discovered that the same inflammatory symptoms in the gut are mirrored in the bone marrow of laboratory animals with inflammatory bowel diseases like colitis and Crohn’s disease. These findings suggest that treatment options could potentially be introduced that directly influence bone marrow function to alleviate symptoms in IBD patients.
Pam Fraker, a distinguished professor of biochemistry and molecular biology at Michigan State University, stated, “It’s possible that if we could reduce bone marrow’s ability to produce inflammatory cells, we could reduce the severity of colitis and Crohn’s disease.” In turn, this could limit the damage caused by these diseases and reduce the number of patients needing surgical interventions.
Understanding Inflammatory Bowel Diseases
To better grasp the potential benefits of targeting bone marrow function in IBD treatment, it’s essential to understand the nature of inflammatory bowel diseases. Colitis and Crohn’s disease are the two most common IBDs, both characterized by chronic inflammation in the digestive tract.
In colitis, the inflammation affects only the inner lining of the colon (the large intestine), whereas, in Crohn’s disease, it involves any part of the gastrointestinal tract and can penetrate deeper layers of the affected tissue. Some of the shared symptoms of these diseases include diarrhea, rectal bleeding, abdominal pain, fatigue, and unintended weight loss.
Limitations of Current Treatment Methods
The current treatments for colitis and Crohn’s disease focus on reducing inflammation and relieving the associated symptoms. However, these therapies can only help manage the diseases rather than actually preventing them or easing their effects. Moreover, as mentioned earlier, these treatments can cause significant degenerative tissue damage, further reducing the quality of life of the patients.
Harnessing Bone Marrow Function to Treat IBDs
The new findings about the relationship between bone marrow and IBD open up exciting research opportunities for developing more effective treatment methods. By focusing on the bone marrow’s ability to produce inflammatory cells, researchers may be able to introduce therapies that can potentially mitigate the symptoms and severity of diseases like colitis and Crohn’s disease.
As a result, this could decrease the number of patients needing steroids, narcotics, or surgical interventions to manage their conditions. Future studies should explore the precise mechanisms by which bone marrow function can be systematically altered and whether these changes can produce the desired outcomes in a clinical setting.
Conclusion
The discovery of the relationship between bone marrow function and inflammatory bowel diseases like colitis and Crohn’s disease is a significant breakthrough in understanding these distressing ailments. By identifying the role of bone marrow in the inflammatory process associated with IBD, new treatment options can be developed that target this vital component, rather than merely managing the symptoms.
By reducing the bone marrow’s ability to produce inflammatory cells, researchers hope to lessen the severity of IBD, limit the damage it causes, and ultimately improve patients’ quality of life. This groundbreaking research will hopefully pave the way for more effective and less invasive treatment options for those living with inflammatory bowel diseases.