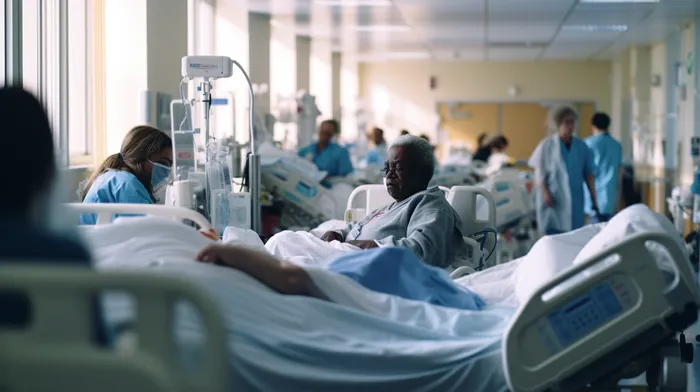
Nobody likes an overcrowded restaurant: long waits, mixed-up orders, and stressed-out waitstaff often lead to an unsatisfactory dining experience. Yet, the same dynamics don’t only apply to restaurants; they are often a reality in hospitals as well. However, in this case, it’s not just a matter of suffering through a less-than-stellar meal, it’s a risk to your health.
Studies conducted at the University of Maryland’s Robert H. Smith School of Business reveal that when hospitals are overwhelmed, surgery patients are sent home before they’re fully recovered. A shocking number of them consequently need to be readmitted to the hospital within three days.
Bed Capacity Dictates Discharge Decisions
According to Bruce Golden, a researcher involved in the University of Maryland study, hospital overcrowding influences discharge decisions. They have found that bed capacity constraints are prioritized over the actual needs of patients, leading to these premature discharges.
Golden emphasizes that hospitals and medical teams must find better solutions than sending patients home too early. He states that too often, hospitals don’t plan ahead, which gets them in trouble with patient traffic jams. Golden suggests that there are logistical strategies hospitals can consider instead of prematurely discharging patients.
Why Do Hospitals Over-Crowd in the First Place?
To understand why hospitals resort to prematurely sending patients home, it’s vital to look at the main contributors to overcrowding in the first place.
- Increased emergency room visits: The number of emergency room (ER) visits has grown significantly in the past few years. More people are relying on ERs for both actual emergencies and non-urgent care. The American College of Emergency Physicians reports that ERs are seeing 130 million patients annually, up from 117 million a decade ago.
-
Lack of bed availability: Hospitals typically operate with a limited number of beds, and if an influx of more severe cases takes up this space, other patients could be asked to leave earlier than they ideally should.
-
Staffing shortages: A lack of qualified doctors, nurses, and other medical personnel can contribute to overcrowding. This situation could put extra strain on existing staff members, leading to stress and fatigue – both of which can impact the quality of patient care.
-
Seasonal fluctuations: Certain times of the year, such as flu season, can lead to a sudden upswing in the demand for hospital care, exacerbating overcrowding.
-
External factors: Unpredictable events such as natural disasters, global pandemics, or mass casualty events can overwhelm hospital resources, including bed availability and staffing, forcing them to discharge patients to make room for new admissions.
The Dangers of Early Discharge
Sending patients home too early can not only be detrimental to their overall health, but it can also increase healthcare costs and hospital readmissions. Some of the risks associated with early discharge include:
- Return visits: If a patient feels unwell or experiences complications after being sent home, they are likely to return to the hospital for more care.
-
Post-operative complications: Surgery can have various short-term and long-term complications, ranging from infections to bleeding or problems related to anesthesia. Sending a patient home too soon increases the risk of these complications going unnoticed.
-
Incomplete healing: An early discharge might result in a patient not receiving the necessary care to fully heal, which can lead to long-term health issues.
-
Increased healthcare costs: Readmissions can lead to higher healthcare costs, both for the patients and the healthcare system.
Moving Forward: Avoiding Overcrowding and Early Discharges
To reduce the negative impact of overcrowding and early discharges, hospitals must implement strategic changes to manage patient flow and improve resource utilization.
- Improve triage procedures: Hospitals can enhance their triage procedures, ensuring that the right patients receive the appropriate level of attention first, and those with less time-sensitive or severe issues follow afterwards.
-
Hire additional staff: By hiring more doctors, nurses, and medical professionals, the quality of patient care can be maintained even when hospitals are crowded.
-
Expand bed capacity: Building additional wards or structures could help alleviate overcrowding and improve the quality of patient care.
-
Implement better patient scheduling systems: Improved scheduling systems that reduce wait times for non-emergency services can lower the burden on emergency rooms and free up beds.
-
Encourage outpatient care: Hospitals can recommend outpatient care when appropriate, which can help to keep patients with minor issues from taking up valuable bed space.
In conclusion, we must not tolerate overcrowded hospitals as a fact of life. As patients, we should advocate for better resource allocation and support hospitals in their efforts to solve this critical issue. This challenge not only impacts overall patient satisfaction but can have life-altering consequences. Investing in strategic solutions to reduce hospital overcrowding and strengthen patient care should be a priority for everyone involved in the healthcare system.